Needle Manipulation in Dry Needling: Three Techniques, Their Mechanisms, and Clinical Consequences
Dry needling has evolved from a rudimentary technique into a sophisticated manual therapy intervention rooted in a comprehensive mechanistic framework. Among the most therapeutically significant aspects of this technique is needle manipulation—specifically, the movement or rotation of a needle after its insertion into tissue. This blog explores the physiological rationale and evidence that supports diverse needle manipulation techniques, including pistoning, winding, and periosteal stimulation. Each technique carries distinct implications for therapeutic outcomes in the practice of dry needling for physical therapy, chiropractic, and athletic training practice.
The Objective of Dry Needling Manipulation
The objective of manual needle manipulation is to improve local, segmental, and systemic responses to dry needling by optimizing mechanical and neurophysiological effects.1-2 Mechanically, manipulation induces microlesions that promote healing, while neurophysiologically, it addresses nociceptive regulation via afferent input. This method stimulates peripheral, spinal, and supraspinal pathways, involving both the somatosensory and autonomic systems. 1-2 These effects occur at multiple levels such as:
- Localized Tissue Effects: Mechanical Disruption and Fibroblast Activation: The manipulation of the needle—via techniques such as pistoning or rotation—exerts mechanical stress on the connective tissue. This stress induces the deformation of collagen fibers and stimulates fibroblasts, which are crucial for tissue repair and remodeling.1,3-4
Biochemical Alterations: Needle manipulation has been demonstrated to modify the biochemical milieu of the targeted tissue. It can specifically diminish levels of nociceptive agents such as substance P and calcitonin gene-related peptide (CGRP), which are linked to pain transmission.4
- Spinal Cord Modulation:
Segmental Inhibition: Mechanical stimulation from needle manipulation activates A-delta and C afferent fibers, which can suppress nociceptive input at the spinal cord level. The segmental inhibition process diminishes the transmission of nociceptive signals to the brain.2
Mitigation of Central Sensitization: Chronic pain disorders frequently entail central sensitization, characterized by an increased sensitivity of the central nervous system to stimuli. Needle manipulation can influence this sensitization by modifying the excitability of dorsal horn neurons in the spinal cord, thereby reducing pain hypersensitivity.1-2,5
- Responses of the Central Nervous System
Activation of Descending Inhibitory Pathways: Needle manipulation stimulates supraspinal areas, such as the periaqueductal gray matter, which activate descending inhibitory pathways. These pathways release endogenous opioids and other neurotransmitters that inhibit pain perception.2
Neuroplastic Changes: Repeated needle manipulation sessions may induce neuroplastic alterations in the brain, hence augmenting the body’s capacity to regulate pain over time. These modifications may yield prolonged analgesia and enhanced functionality.6
Clinical Consequences
Comprehending needle manipulation’s diverse impacts highlights its significance in dry needling therapy. Needle manipulation effectively manages musculoskeletal pain and dysfunction by engaging local tissues, regulating spinal cord activity, and eliciting reactions from the central nervous system.
Dry Needling Pistoning: Inducing Twitch Responses and Localized Lesions
The dry needling pistoning technique, defined by swift in-and-out needle movements, is typically utilized to deactivate myofascial trigger points (MTrPs). This assertive technique seeks to provoke local twitch responses (LTRs), which are thought to be associated with enhanced pain results. Recent study, however, has called into doubt the necessity and reliability of this technique.7
Perreault et al. (2019) examined studies indicating that although LTRs are a prevalent clinical focus, they do not significantly correspond with enhanced short-term outcomes in patients experiencing neck, shoulder, or low back pain. Furthermore, excessive pistoning may exacerbate post-needling discomfort and inflammatory reactions, prompting concerns of overtreatment. Histological research indicates that recurrent mechanical damage near neuromuscular connections may offer no further advantage and could instead lead to detrimental tissue responses.1
Moreover, the inter-examiner reliability in identifying MTrPs has been proved inadequate, compromising the clinical accuracy of pistoning-based methodologies. The literature increasingly advocates for a more comprehensive understanding of dry needling that extends beyond myofascial trigger point deactivation, highlighting alternative manipulation approaches that yield more consistent therapeutic outcomes.7
Winding: Mechanotransduction and Modulation of Connective Tissue
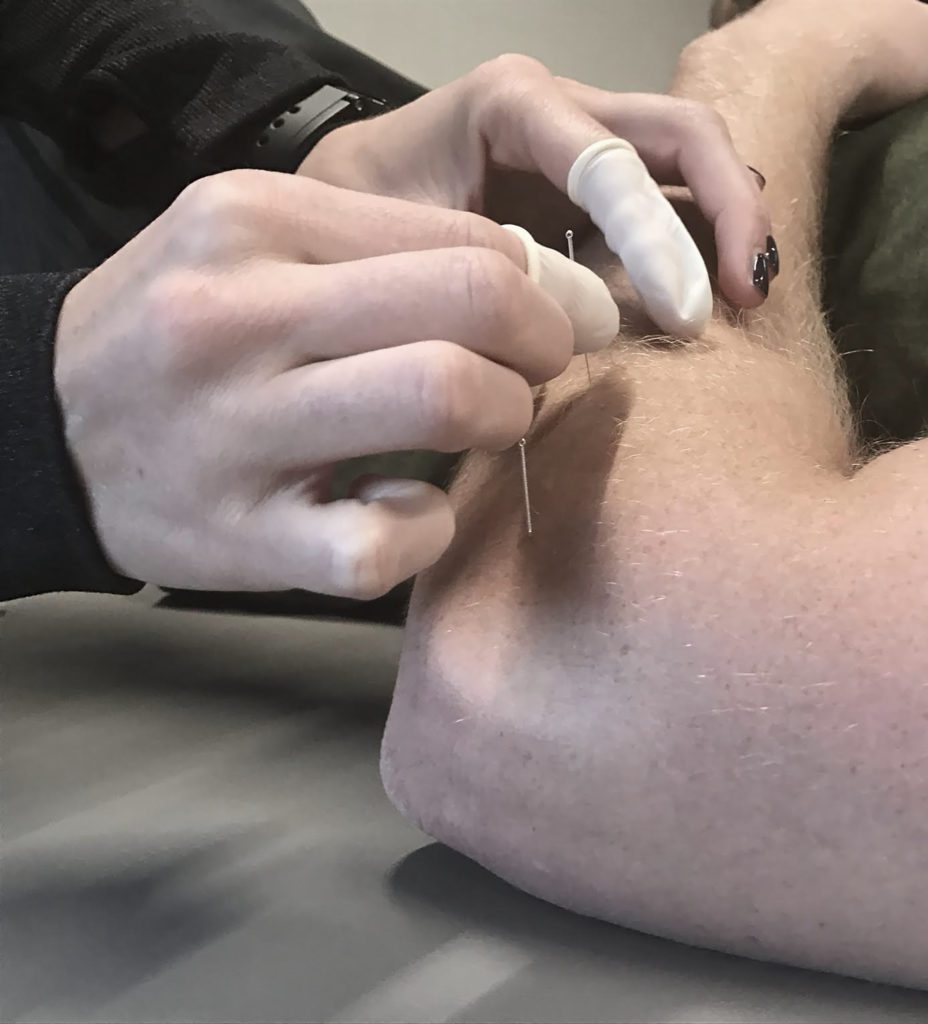
Unlike pistoning, needle winding—the rotational manipulation of an indwelling needle—concentrates on interacting with the connective tissue matrix. This method is well-supported by both fundamental research and clinical literature. Winding establishes a mechanical connection between the needle and the extracellular matrix, facilitating the transmission of force to fibroblasts and sensory neurons by mechanotransduction.1
Langevin et al. established that tissue around a rotating needle enhances pullout force, a phenomenon referred to as “needle grasp,” which is associated with the deformation of collagen fibers and the activation of afferent C and Aδ fibers. These afferents trigger pain-modulating responses at both the spinal cord and supraspinal levels. This mechanical signal induces cellular alterations, such as fibroblast realignment and modification of extracellular matrix proteins, which may improve tissue repair.3
Further research has demonstrated that winding manipulation triggers mast cell degranulation, resulting in the localized release of histamine, adenosine, and ATP. These neurochemical mediators stimulate purinergic and histaminergic receptors, hence modulating nociceptive signals. Adenosine specifically binds to A1 receptors in the dorsal horn, facilitating the release of endogenous opioids and segmental pain inhibition.1-3
The De Qi response—characterized by an aching or heavy sensation while winding—is linked to limbic and subcortical deactivation observed in fMRI, indicating a significant central component to the analgesic effects of this treatment. In contrast to pistoning, winding seems to offer both localized tissue modulation and systemic pain relief without the inflammatory dangers involved.1
Periosteal Stimulation: Focusing on the Sclerotome for Osseous Pain
Periosteal pecking is a specific technique of needle manipulation designed to activate bone-related nociceptors via direct interaction with the periosteum. This method focuses on segmentally innervated osseous structures (sclerotomes) and is particularly pertinent in addressing ailments such as knee osteoarthritis (OA).8-10
Weiner et al. executed a randomized controlled trial on periosteal stimulation for advanced knee osteoarthritis, revealing that subjects subjected to needling of bony structures with electrical stimulation experienced a substantial reduction in pain over nine months, especially when booster treatments were incorporated. Dunning et al. similarly discovered that the integration of periosteal electrical dry needling into an osteoarthritis rehabilitation program yielded superior pain alleviation and functional enhancements relative to manual therapy and exercise alone.8 It is not a knee specific effect however as it can be used in other areas as well.8-11
Animal models corroborate these findings at the cellular level. Periosteal stimulation has been demonstrated to regulate collagen metabolism, diminish cartilage breakdown, and enhance the expression of anti-inflammatory cytokines. The biological results underscore that periosteal needling influences both nociceptive pathways and the pathophysiological mechanisms associated with chronic joint disorders.12-13
Comparative Analysis and Clinical Applications
A prevalent theme in contemporary studies indicates that the intensity and methodology of needle manipulation significantly influence therapeutic outcomes. Although historically significant in the treatment of myofascial trigger points (MTrP), pistoning is currently subject to re-evaluation owing to inconsistent results and insufficient diagnostic reliability. Conversely, winding and periosteal procedures exhibit substantial mechanical and biochemical effects, as corroborated by both human and animal research.
From a clinical standpoint, manipulation must correspond to the targeted tissue and the intended physiological response. For instance:
- Winding is effective for improving local tissue regeneration and beginning systemic pain regulation, especially in persistent myofascial disorders.
- Pistoning may be advantageous in meticulously chosen instances where myofascial trigger points are distinctly recognized as the principal sources of discomfort.
- Periosteal stimulation is increasingly recognized as an effective approach for alleviating segmentally mediated osseous pain, particularly when combined with electrical stimulation.
Conclusion: Integrating Dry Needling Manipulation into Precision Dry Needling Practice
The aggregate evidence derived from histological, neurophysiological, and clinical studies underscores the significance of needle manipulation as a fundamental factor in the efficacy of dry needling. Beyond mere mechanical puncture, procedures such as pistoning, winding, and periosteal pecking activate specific biological pathways that influence tissue repair, neuromodulation, and pain perception.
Rotation-based treatments, particularly needle winding, appear to yield enhanced outcomes by stimulating the connective tissue matrix and initiating mechanotransduction, which subsequently activates mast cells, fibroblasts, and sensory afferents. These processes culminate in localized tissue remodeling, improved perfusion, and the regulation of peripheral and central sensitization through adenosine- and opioid-mediated pathways. Furthermore, imaging and biochemical investigations reveal that winding not only impacts local tissues but also modifies brain activity and descending pain regulation, as evidenced by fMRI and CSF neuropeptide analyses.
Conversely, pistoning retains its utility in certain therapeutic contexts, particularly when an active myofascial trigger point is consistently identified as the primary source of pain. Nevertheless, its excessive utilization or indiscriminate application is under scrutiny due to concerns regarding potential tissue damage, post-needling discomfort, and insufficient inter-examiner reliability in identifying myofascial trigger points.
Periosteal stimulation, especially when integrated with electrical currents, represents a novel strategy for the management of sclerotomal pain and osteoarthritic conditions by engaging segmental spinal processes and influencing intra-articular biochemistry. This technique further emphasizes the importance of precise needle manipulation tailored to anatomical and neurophysiological objectives.
The Path Forward
As our understanding of manual needle stimulation expands, it becomes evident that precision, rather than tradition, should guide dry needling practices. Clinicians must move beyond a “one-technique-fits-all” mentality and adopt a mechanism-driven approach, selecting the manipulation technique that most closely aligns with the patient’s pathophysiology, tissue type, and therapeutic goals.
Future research should concentrate on optimizing dose parameters, including manipulation intensity, duration, and frequency, while also identifying patient-specific factors influencing response. Comprehensive randomized trials and mechanistic studies will clarify the role of needle manipulation in various musculoskeletal and neurological disorders.
In conclusion, needle manipulation is not ancillary—it is essential. When executed with intention and supported by scientific evidence, dry needling transforms from a mere procedural intervention into a precise therapeutic modality that addresses the underlying causes of complex pain and movement disorders. If you are a practitioner that wants to learn dry needling you can find foundations courses near you courses, enroll in an open course today at www.structureandfunction.net.
References
- Perreault T, Grubb MT, Gendron BC, and colleagues. Mechanisms and Dosage Parameters of Manual Needle Stimulation: Clinical Considerations – Part 2. Acupuncture in Physical Therapy. 2019;31(1):9–23.
- Butts, Raymond, and James Dunning. “Peripheral and Spinal Mechanisms of Pain and Dry Needling Mediated Analgesia: A Clinical Resource Guide for Health Care Professionals.” International Journal of Physical Medicine & Rehabilitation 04, no. 02 (2016). https://doi.org/10.4172/2329-9096.1000327.
- Langevin HM, Churchill DL, Wu J, et al. Evidence of connective tissue involvement in acupuncture. FASEB Journal. 2002;16(8):872–874.
- Langevin HM, et al. Biomechanical reaction to acupuncture needling in humans. Journal of Applied Physiology. 2001;91(6):2471–2478.
- Hsieh YL, et al. Biochemical alterations in the dorsal horn and cerebrospinal fluid following dry needling. Journal of Pain. 2012;13(5):505–515.
- Asghar A, Green G, Lythgoe MF, et al. Acupuncture influences limbic and subcortical brain regions. Journal of Neuroscience Research. 2010; Volume 88, Issue 4, Pages 822–831.
- Dunning J., Butts R., Mourad F., et al. A literature review on dry needling with implications for clinical practice guidelines. Physical Therapy Reviews. 2014;19(4):252–265.
- Weiner DK, et al. Periosteal stimulation for knee osteoarthritis: a randomized controlled trial. Journal of the American Geriatrics Society. 2013;61(6):985–992.
- Kaye, Alan D., Olivia Mipro, Brynne E. Tynes, Brennan Abbott, Caylin Roberts, Jelena Vučenović, Kyle Jenks, et al. “Periosteal Electrical Dry Needling Efficacy in Knee Osteoarthritis: A Systematic Review.” Current Pain and Headache Reports 29, no. 1 (February 15, 2025): 48. https://doi.org/10.1007/s11916-025-01362-7.
- Dunning, James, Raymond Butts, Ian Young, Firas Mourad, Victoria Galante, Paul Bliton, Michelle Tanner, and César Fernández-de-las-Peñas. “Periosteal Electrical Dry Needling as an Adjunct to Exercise and Manual Therapy for Knee Osteoarthritis: A Multi-Center Randomized Clinical Trial.” The Clinical Journal of Pain, May 2018, 1. https://doi.org/10.1097/AJP.0000000000000634.
- Staehli Wiser, Anna, James Dunning, Casey Charlebois, Paul Bliton, and Firas Mourad. “Periosteal Dry Needling for Carpometacarpal Osteoarthritis: A Prospective Case Series.” Journal of Clinical Medicine 12, no. 17 (August 31, 2023): 5678. https://doi.org/10.3390/jcm12175678.
- Shi X, Yu W, Wang T, et al. Electroacupuncture alleviates cartilage degradation: Improvement in cartilage biomechanics via pain relief and potentiation of muscle function in a rabbit model of knee osteoarthritis. Biomedicine & Pharmacotherapy. 2020;123:109724. doi:10.1016/j.biopha.2019.109724
- Shi G-X, Tu J-F, Wang T-Q, et al. Effect of Electro-Acupuncture (EA) and Manual Acupuncture (MA) on Markers of Inflammation in Knee Osteoarthritis. JPR. 2020;Volume 13:2171-2179. doi:10.2147/JPR.S256950