Physiologic Perspective on the Local Effects of Dry Needling
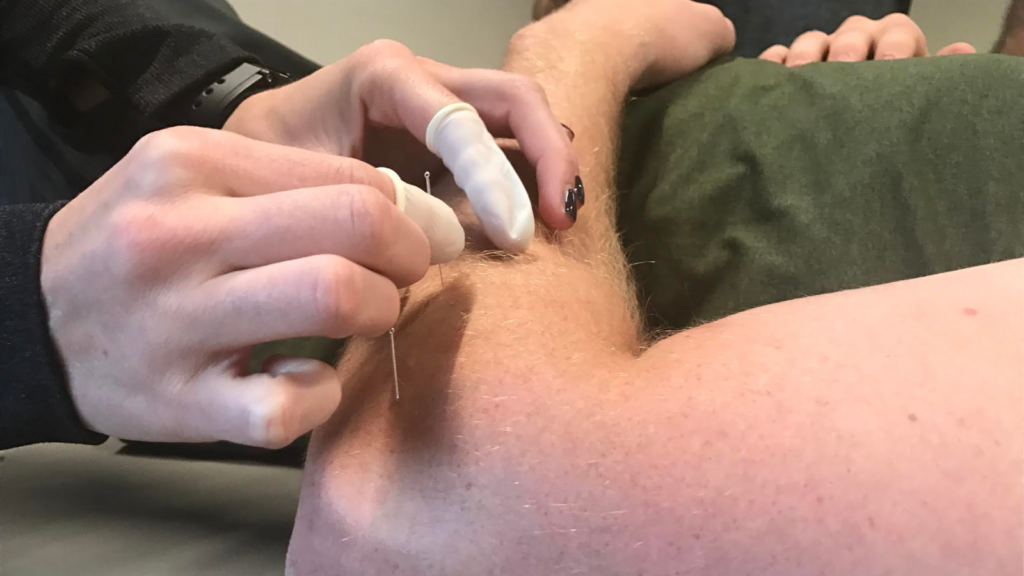
Dry needling is a powerful tool that physical therapists, athletic trainers, and chiropractors can utilize to address musculoskeletal pain and dysfunction. While teaching dry needling courses for Structure & Function Education®, one of the most common questions I get is how dry needling works. Dry Needling is a technique that involves inserting thin, monofilament needles into myofascial trigger points, scar tissue, or other dysfunctional soft tissues. While the benefits of dry needling are often discussed in broader terms, understanding the local physiological effects is crucial for clinicians who want to maximize the therapeutic outcomes for their patients. This blog delves into the science behind the regional effects of dry needling and how these mechanisms translate into improved patient care.
The Local Effects of Dry Needling: A Deep Dive into Physiological Mechanisms
Dry needling, a technique widely embraced by physical therapists, athletic trainers, and chiropractors, is more than just a pain relief method. It is an intervention that taps into the body’s innate physiological processes to promote healing and restore function. By inserting thin needles into specific myofascial trigger points, scar tissue, or other dysfunctional areas, clinicians can trigger a cascade of local physiologic effects that have profound implications for patient care1.
The complexity of dry needling’s effects lies in the varied physiological responses dry needling lesions create. These lesions ultimately influence the body’s inflammatory processes, reducing pain, improving tissue function, and enhancing mobility and the ability to load. Let’s explore these local effects of dry needling, focusing on how these mechanisms work at the tissue level and their impact on patient outcomes.
Neurochemical Release: Using the Body’s Natural Painkillers
When a needle penetrates the skin and reaches a dysfunctional area, it doesn’t sit idly. It activates a neurochemical response. Opioids and Monomines—two potent pain-relieving compounds—are released2–4. These neurochemicals bind to receptor sites in the central and peripheral nervous systems, creating a localized analgesic effect. Pain signals are muted through this process, providing pain relief for patients.
However, this relief is only uniform across some patients. The body’s response can vary, creating complexity in how individuals experience pain reduction. For some, the effect is almost instantaneous, while for others, the process is more gradual. The release of substance P and adenosine adds another layer of complexity. Though they are involved in pain transmission, their presence also kickstarts an inflammatory response, which is vital for tissue repair5–7.
The dual roles of substance P and adenosine—promoting pain and healing—illustrate the intricacies of dry needling. It’s a process that’s as much about initiating an inflammatory process that will lead to healing as it is about pain management and understanding these nuances is crucial for any clinician using this technique. This is why taking a dry needling course from Structure & Function Education® is essential, as students’ understanding of these effects is a primary focus of our curricula.
Microtrauma and Tissue Remodeling: A Healing Process
Dry needling does more than alter neurochemistry; it also induces microtrauma. This microtrauma, though minimal, is enough to trigger the body’s natural healing processes. The needle creates small lesions within the tissue, which prompts the body to heal the lesions in the area 8–11.
The body responds to these “lesions” by sending fibroblasts to the area. These cells are responsible for producing collagen, a protein crucial for tissue repair and regeneration. Collagen is not just any protein; it is the primary building block of the extracellular matrix, the framework that provides structure to tissues. The extracellular matrix is remodeled through collagen synthesis and deposition, which has been discussed as the mechanotransductive effect of dry needling8,12,13.
This remodeling is particularly significant for patients with chronic conditions, such as dense scar tissue or long-standing myofascial pain. For example, in scar tissue, collagen fibers are often disorganized, leading to stiffness and pain. The microtrauma from dry needling can disrupt this disorganization, allowing the body to replace it with healthier, more aligned fibers. This process can significantly improve tissue function, reduce scar pain, and enhance scar mobility14–16.
The implications of this for patient care are profound. For clinicians, dry needling can be more than a temporary pain relief technique—it can be a pathway to lasting tissue health. However, the effectiveness of this process depends on the precise application of the method, which is why proper training in dry needling courses like that provided by Structure & Function Education® is essential.
Targeting Specific Tissues: The Precision of Dry Needling
The success and safety of dry needling hinges on precision. The technique is not a one-size-fits-all solution; it requires a deep understanding of the anatomy and the underlying pathology17–19. This is where clinical decision-making comes into play. Clinicians must assess each patient’s unique presentation and determine the exact location and depth for needle insertion.
Trigger point dry needling is a prime example of this precision20,21. Trigger points are hyperirritable spots within a taut band of muscle that can refer pain to other areas. Releasing these points can provide immediate pain relief and restore muscle function. However, the effectiveness of this release depends on hitting the right spot at the correct depth and using the proper technique.
Similarly, dry-needling scar tissue requires a different approach. Scar tissue, particularly after surgery or injury, can become thick and fibrous, restricting movement and causing discomfort. By carefully targeting this tissue, clinicians can stimulate the breakdown of the fibrous tissue, promoting the production of new, healthier collagen. This process can enhance flexibility, reduce pain, and improve overall function.
Proper technique is the cornerstone of effective dry needling, best achieved through comprehensive training. Structure & Function Education’s® dry needling courses equip clinicians with the skills and knowledge to perform this technique safely and effectively, ensuring that patients benefit most.
Enhancing Clinical Practice: Practical Implications
Incorporating dry needling into clinical practice offers numerous benefits. For one, it allows for a more targeted approach to treating musculoskeletal pain and dysfunction. By understanding the local effects of dry needling, clinicians can tailor their interventions to address each patient’s specific needs21.
For instance, athletes recovering from injury can benefit from dry needling as part of their rehabilitation. The technique helps reduce pain and promotes tissue repair, allowing athletes to return to their sport more quickly and with less risk of re-injury. Similarly, patients with chronic pain conditions can experience significant relief and functional improvement, thanks to the tissue remodeling effects of dry needling.
Furthermore, dry needling is a versatile tool that can be integrated into a comprehensive treatment plan. Whether combined with manual therapy, exercise, or other interventions, dry needling can enhance the overall effectiveness of patient care.
Conclusion: The Importance of Dry Needling Courses
Understanding and effectively applying the local effects of dry needling requires both knowledge and skill. For clinicians looking to expand their expertise, enrolling in a dry needling course is an invaluable investment. These courses provide in-depth training on the physiological mechanisms of dry needling and hands-on experience in applying the technique. To find a Structure & Function Education® dry needling course, enroll today in the Foundations in Dry Needling for Orthopedic Rehab & Sports Performance course at structureandfunction.net. Sign up today and gain the confidence and competence to use this powerful modality in their practice. This improves patient outcomes and enhances the clinician’s ability to provide comprehensive, evidence-based care.
In the end, the value of dry needling lies in its ability to address both the symptoms and underlying causes of musculoskeletal pain and dysfunction. For clinicians committed to providing the highest level of care, mastering dry needling through dedicated courses is essential.
References
- Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic Effects of Dry Needling. Curr Pain Headache Rep. 2013;17(8):348. doi:10.1007/s11916-013-0348-5
- Butts R, Dunning J. Peripheral and Spinal Mechanisms of Pain and Dry Needling Mediated Analgesia: A Clinical Resource Guide for Health Care Professionals. Int J Phys Med Rehabil. 2016;04(02). doi:10.4172/2329-9096.1000327
- Perreault T, Grubb MT, Gendron BC, Perez JC, Flannagan SO. Mechanisms and Dose Parameters of Manual Needle Stimulation: Clinical Considerations – Part 2. Acupunct Physiother. Published online 2019:15.
- Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85(4):355-375. doi:10.1016/j.pneurobio.2008.05.004
- Goldman N, Chen M, Fujita T, et al. Adenosine A1 receptors mediate the local anti-nociceptive effects of acupuncture. Nat Neurosci. 2010;13(7):883-888. doi:10.1038/nn.2562
- Liao HY, Hsieh CL, Huang CP, Lin YW. Electroacupuncture Attenuates CFA-induced Inflammatory Pain by suppressing Nav1.8 through S100B, TRPV1, Opioid, and Adenosine Pathways in Mice. Sci Rep. 2017;7(1):42531. doi:10.1038/srep42531
- Zhang R yi, Zhu B fan, Wang L kui, et al. Electroacupuncture alleviates inflammatory pain via adenosine suppression and its mediated substance P expression. Arq Neuropsiquiatr. 2020;78(10):617-623. doi:10.1590/0004-282×20200078
- Langevin HM, Bouffard NA, Badger GJ, Churchill DL, Howe AK. Subcutaneous tissue fibroblast cytoskeletal remodeling induced by acupuncture: Evidence for a mechanotransduction-based mechanism. J Cell Physiol. 2006;207(3):767-774. doi:10.1002/jcp.20623
- Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol. 2001;91(6):2471-2478. doi:10.1152/jappl.2001.91.6.2471
- Langevin HM, Churchill DL, Cipolla MJ. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB J Off Publ Fed Am Soc Exp Biol. 2001;15(12):2275-2282. doi:10.1096/fj.01-0015hyp
- Langevin HM. Acupuncture, connective tissue, and peripheral sensory modulation. Crit Rev Eukaryot Gene Expr. 2014;24(3):249-253.
- de Almeida M dos S, Guerra FDR, de Oliveira LP, Vieira CP, Pimentel ER. A Hypothesis for the Anti-Inflammatory and Mechanotransduction Molecular Mechanisms Underlying Acupuncture Tendon Healing. Acupunct Med. 2014;32(2):178-182. doi:10.1136/acupmed-2013-010455
- Yao W, Yang H, Yin N, Ding G. Mast Cell-Nerve Cell Interaction at Acupoint: Modeling Mechanotransduction Pathway Induced by Acupuncture. Int J Biol Sci. 2014;10(5):511-519. doi:10.7150/ijbs.8631
- Rozenfeld E, Sapoznikov Sebakhutu E, Krieger Y, Kalichman L. Dry needling for scar treatment. Acupunct Med. Published online March 30, 2020:096452842091225. doi:10.1177/0964528420912255
- Bahramian M, Dabbaghipour N, Aria A, Sajadi moghadam fard tehrani B, Dommerholt J. Efficacy of Dry Needling in Treating Scars following Total Hip Arthroplasty: A Case Report. Med J Islam Repub Iran. 2022;36:156. doi:10.47176/mjiri.36.156
- Trybulski R, Kawczyński A, Muracki J, Lovecchio N, Kużdżał A. Dry Needling and Acupuncture for Scars—A Systematic Review. J Clin Med. 2024;13(14):3994. doi:10.3390/jcm13143994
- Halle JS, Halle RJ. PERTINENT DRY NEEDLING CONSIDERATIONS FOR MINIMIZING ADVERSE EFFECTS – PART ONE. :12.
- Halle JS, Halle RJ. PERTINENT DRY NEEDLING CONSIDERATIONS FOR MINIMIZING ADVERSE EFFECTS – PART TWO. :10.
- Peuker E, Cummings M. Anatomy for the Acupuncturist – Facts & Fiction. Acupunct Med.:9.
- Dommerholt J. Dry needling — peripheral and central considerations. J Man Manip Ther. 2011;19(4):223-227. doi:10.1179/106698111X13129729552065
- Dommerholt J, Fernández-de-las-Peñas C, Petersen SM. Needling: is there a point? J Man Manip Ther. 2019;27(3):125-127. doi:10.1080/10669817.2019.1620049