From Needles to Healing: Understanding the Role of Dry Needling in Modulating Pain and Inflammation
As an athletic trainer with extensive expertise in dry needling, I have observed the significant potential of this therapeutic technique to improve recovery outcomes for both athletes and patients. Dry needling has been recognized as an effective therapeutic intervention for musculoskeletal conditions, primarily due to its capacity to reduce inflammation and pain, as highlighted by Butts et al.1 Nevertheless, the mechanisms underlying its effectiveness extend well beyond the simple disruption of myofascial trigger points. Instead, it influences pain and inflammation at both peripheral and central levels through a complex interaction of biochemical, biomechanical, endocrinological, and neurovascular processes. Consequently, understanding these multifaceted mechanisms is essential for optimizing their application in sports medicine and physical therapy. Understanding dry needling in modulating pain and inflammation opens the door to multiple treatment approaches.
Overview of Dry Needling in Modulating Pain and Inflammation
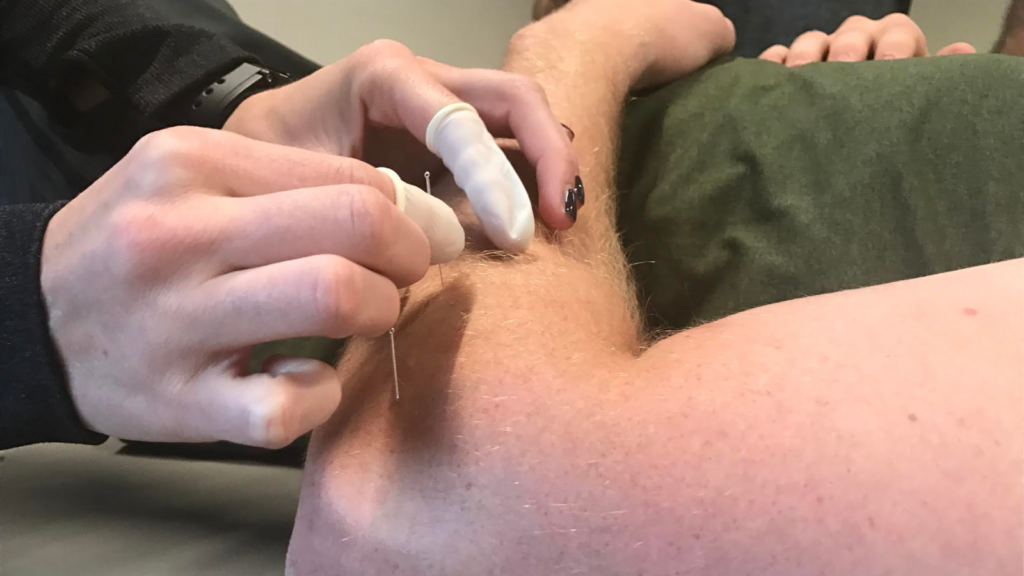
Dry needling has become a prominent technique in sports medicine; however, what sets it apart from other interventions? Dry needling mainly involves inserting thin, filament needles into muscles, ligaments, tendons, and near nerves to reduce pain and improve function. It is often used for myofascial pain, sports injuries, and various musculoskeletal conditions. Although it may look similar to acupuncture, it is based on the principles of Western medicine’s anatomy and physiology. Dry needling mainly targets muscles, ligaments, tendons, and nearby nerves, which are believed to cause pain and dysfunction. The goal is to restore normal muscle function and lessen soreness by stimulating the body’s natural immune system and healing processes. Having a better understanding of the use of dry needling in modulating pain and inflammation will benefit the clinician making clinical decisions on treatment and care progression.
Physiological Mechanisms
The insertion of fine needles into targeted tissues initiates a cascade of physiological responses, influencing pain perception and inflammatory processes. A crucial element is the regulation of the local inflammatory response. Studies suggest that dry needling may modify the concentrations of significant pro-inflammatory and anti-inflammatory cytokines. For instance, it has been demonstrated to reduce levels of substance P and calcitonin gene-related peptide, both of which are linked to pain and inflammation.2 However, trigger points are not the sole factor. It is essential to acknowledge that dry needling activates the body’s intrinsic analgesic mechanisms, releasing endocannabinoids and engaging the sympathetic nervous system (SNS) to produce pain-relieving chemicals. Furthermore, it extends its effects to the non-opioid pathway, facilitating the release of serotonin and norepinephrine from the brainstem—thereby providing enhanced analgesia.1
Butts et al. have demonstrated that dry needling can activate both opioid and non-opioid pain reduction pathways, which are mediated by endogenous cannabinoids, serotonin, and norepinephrine, in addition to its local effects.1 This modulation also occurs via the hypothalamic-pituitary-adrenal (HPA) axis, which can inhibit COX-2 and reduce inflammatory cytokines.1,3 Dry needling can reverse peripheral hyperalgesic priming by normalising nociceptive channels, such as TRPV, ASIC, TTX, and P2X/Y.1,3 Additionally, TRPV1 and P2X/Y activate mechanotransduction processes in fibroblasts and peripheral nerves, impacting the transmission of spinal pain and the propagation of intracellular calcium waves.
Furthermore, dry needling may facilitate the release of endogenous opioids, which inhibit pain signals at the spinal cord level.4 Additionally, it activates the hypothalamic-pituitary-adrenal (HPA) axis, serving as the regulatory center for the body’s stress response.3 This neurophysiological response is crucial for disrupting the chronic pain cycle, promoting muscle relaxation, and enhancing blood circulation to the affected region, thereby supporting effective inflammatory management. Such stimulation induces intracellular calcium wave propagation, affecting spinal pain transmission.1 Moreover, the release of histamine from needling offers an additional benefit in pain management away from the site of irritation.1-3
What Does the Research Say about Dry Needling in Modulating Pain and Inflammation?
Initial investigations have begun to elucidate how dry needling may function as a valuable adjunct to traditional therapy for reducing inflammation. A randomized controlled trial examined the effects of dry needling on patients with myofascial pain syndrome and demonstrated significant reductions in inflammatory markers post-treatment compared to a sham control.5 Alternatively, a study involving athletic populations with shoulder injuries revealed improved inflammatory outcomes, range of motion, and pain.6 Additionally, functional Magnetic Resonance Imaging (fMRI) studies have established that acupuncture stimulation correlates with specific neural responses, indicating dry needling in modulation of pain and inflammation pathways within the brain.3
Electrical Dry Needling (EDN) has been shown to induce immune cells, fibroblasts, and keratinocytes to secrete calcitonin gene-related peptide (CGRP) and substance P.1 This mechanism relates to increased nerve receptor sensitivity, and reversing this process may promote improved recovery. Magnetic Resonance Imaging (MRI) and ultrasound examinations have substantiated these findings, illustrating reduced edema and hyperemia in the specific muscle regions following treatment with dry needling.7 These objective measurements provide compelling evidence of the technique’s impact on inflammatory mechanisms at a physiological level. EDN has the capacity to stimulate the supraoptic nucleus to secrete oxytocin.1 This process can diminish hyperactive peripheral pain receptors while concurrently activating spinal opioid interneurons.
Consequences for Athletic Training
The incorporation of dry needling into rehabilitation programs offers athletic trainers two primary advantages: relief from pain and enhanced management of inflammation. It is important to recognize that its application extends beyond mere trigger points. Consider the broader context of dry needling for modulating pain and inflammation. This approach is particularly advantageous in high-pressure environments such as competitive sports, where rapid recovery from injuries is essential. Do not hesitate to utilize electrical stimulation alongside dry needling, as it may be instrumental in achieving more significant benefits, especially in cases of chronic pain. Integrating dry needling into a comprehensive therapeutic regimen enables trainers to improve athletes’ performance and health outcomes.
Prospective Trajectories in Dry Needling In Modulating Pain and Inflammation
Future research is essential to deepen our understanding of the specific mechanisms through which dry needling influences inflammation. Advances in imaging techniques and molecular biology hold promise for uncovering new insights into this complex relationship. The future may also yield novel information concerning remote anatomical sites. Dry needling in modulating pain and inflammation is an important topic and more research is warranted.
Progress in these fields is anticipated to enhance and expand the therapeutic applications of dry needling within clinical and athletic settings. It is vital to comprehend the most effective integration of manual and electrical stimulation methods. Key questions include: Understanding the dose-response relationships for DN for various conditions? Additionally, how might individual physiological factors, such as genetics, hormone levels, and stress, affect the effectiveness of dry needling?
In conclusion, dry needling constitutes a synthesis of traditional techniques and modern research, offering innovative strategies for managing inflammation and promoting recovery. As ongoing investigations explore its full capabilities, its importance in pain management and rehabilitation is anticipated to expand, ultimately benefiting both athletes and non-athletes. Dry needling involves more than the simple insertion of needles into trigger points; it seeks to activate the body’s innate healing potential. The use of dry needling in modulating pain and inflammation is a topic for continued investigation. Continually seek knowledge, question all sources, and uphold a spirit of inquisitiveness. If you are a practitioner that wants to learn dry needling, you can find foundation courses near you; enroll in an open course today at www.structureandfunction.net.
References
- Butts, R., Dunning, J., Perreault, T., Mourad, F., & Grubb, M. (2016). Peripheral and Spinal Mechanisms of Pain and Dry Needling Mediated Analgesia: A Clinical Resource Guide for Healthcare Professionals. International Journal of Physical Medicine & Rehab .
- Dommerholt, Jan. “Dry Needling — Peripheral and Central Considerations.” Journal of Manual & Manipulative Therapy 19, no. 4 (November 2011): 223–27. https://doi.org/10.1179/106698111X13129729552065.
- Cho, Z. H., Hwang, S. C., Wong, E. K., Son, Y. D., Kang, C. K., Park, T. S., Bai, S. J., Kim, Y. B., Lee, Y. B., Sung, K. K., Lee, B. H., Shepp, L. A., & Min, K. T. (2006). Neural substrates, experimental data, and functional hypotheses about the processe
- Gunn CC. The Gunn methodology for addressing chronic pain: intramuscular stimulation for myofascial pain of radiculopathic origin. Elsevier Health Sciences; 1996.
- Tekin, Levent, Selim Akarsu, Oğuz Durmuş, Engin Çakar, Ümit Dinçer, and Mehmet Zeki Kıralp. “The Effect of Dry Needling in the Treatment of Myofascial Pain Syndrome: A Randomized Double-Blinded Placebo-Controlled Trial.” Clinical Rheumatology 32, no. 3 (Mhttps://doi.org/10.1007/s10067-012-2112-3.
- Ceballos-Laita L, Medrano-de-la-Fuente R, Estébanez-De-Miguel E, Moreno-Cerviño J, Mingo-Gómez MT, Hernando-Garijo I, Jiménez-Del-Barrio S. Effects of Dry Needling in Teres Major Muscle in Elite Handball Athletes. A Randomised Controlled Trial. J Clin Med
- Tekin L, et al. The impact of dry needling on myofascial pain syndrome treatment: a comparative analysis with alternative physical therapy methods. Am J Phys Med Rehabil. 2013;92(1):88-96.