A recent publication has provided insight into one of the rationales for dry needling we discuss in our courses, treating scars1. Scarring of the skin affects millions of patients and in sports medicine, we often deal with post-surgical scars with our patients. An estimated 100 million patients per year acquire scars from surgery in the developed world2. In the United States, chronic wounds affect around 6.5 million patients3. According to the latest data from the National Center for Health Statistics, 40 million inpatient surgical procedures were performed in the United States in 2000, followed closely by 31.5 million outpatient surgeries3. The need for post-surgical wound care is sharply on the rise. Patients with visible scars, particularly on the face, suffer from social stigma and psychological trauma2,4. There are many treatments for scarring available, and there is an estimated $12 billion annual market in the United States for scar treatment3.
Wound healing is a complex process that encompasses four stages: hemostasis, inflammation, proliferation, and remodeling. If this process is altered, it can cause scarring (hypertrophic, keloid or atrophic scars)5-7. Dry needling can be used to influence this process in several helpful ways. The local biomechanical, chemical and vascular effects of needling have been well documented. Improved circulation and prompting of the body’s inflammatory processes have been demonstrated following dry needling8. Additionally, we know the mechanotransductive processes that occur locally influencing the tissues. A series of recent studies by Langevin et al., describes what is occurring during mechanotransduction and the mechanism’s involved9-14. These articles suggest that needle grasp results when collagen fibers and other tissues wind around the rotating needle10-14. The tissues experience significant deformation during this process and induce a remodeling by fibroblastic activity13-14. Thus, this mechanotransductive mechanism is driven by tissue deformation through needle manipulation that can mechanically stimulate fibroblasts for therapeutic benefits9-11. These ideas were also verified by Julias et al. who explored this link between tissue properties and collagen fiber winding15. Thus, using dry needles to manipulate the scar makes sense physiologically.
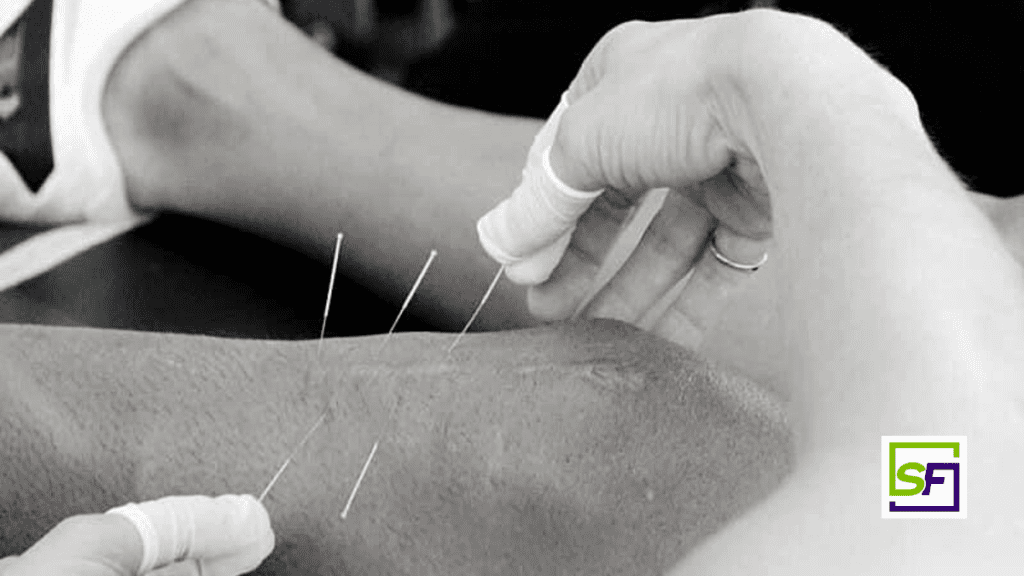
This article was interesting in that it detailed the procedure for treating scars with dry needling. It outlines an old acupuncture technique known as “surrounding the dragon” that involves encircling the problem area with needles1. They reviewed a few studies and came up with a protocol which is exactly what we discuss in our foundation’s course. They suggest the following protocol for scar needling.
- Needles (0.25 mm ~ 30 mm) should be placed along the entire scar spaced 0.5–1.0 cm from one another.
- Needles should be inserted at a distance of 0.5–1.0 cm from the scar, angled 30–45° toward the scar.
- The retention time should be ~20 min. Needle twisting may be added depending on the patient’s sensitivity.
- They suggest the treatment should be performed once or twice a week until resolution or a symptom plateau is achieved.
Conclusion
In addition to the article reviewed above, there is additional evidence of these effects on hypertrophic scars7. A comprehensive discussion of these mechanisms and responses to the mechanical stimulus of dry needling can be found in Perreault et al16. This information informs how we use dry needling for the purposes of healing and remolding of scars. If you’re interested in learning how Structure & Function Education’s Pentamodal Method of dry needling can be used to manipulate scars, enroll in the SFDN1 – Foundations in Dry Needling for Orthopedic Rehab & Sport Performance course at www.structureandfunction.net.
Brian V. Hortz, Ph.D., AT, SFDN
Director of Research and Education – Structure & Function Education
References
- Rozenfeld, Evgeni, Eleanora Sapoznikov Sebakhutu, Yuval Krieger, and Leonid Kalichman. “Dry Needling for Scar Treatment.” Acupuncture in Medicine, March 30, 2020, 096452842091225. https://doi.org/10.1177/0964528420912255.
- Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthetic Surg 2008;61:1049–1058
- Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17(6):763–771. doi:10.1111/j.1524-475X.2009.00543.x
- Hunt O, Burden D, Hepper P. Stevenson M. Johnston C. Self-reports of psychosocial functioning among children and young adults with cleft lip and palate. Cleft Palate Craniofac J 2006;43:598–605.
- Bordoni B and Zanier E. Skin, fascias, and scars: symptoms and systemic connections. J Multidiscip Healthc 2013; 7: 11–24.
- Fang S. The successful treatment of pain associated with scar tissue using acupuncture. J Acupunct Meridian Stud 2014; 7(5): 262–264
- Song, Haiyun, Jingping Mu, and Jun Wang. “Clinical Study on Treatment of Hypertrophic Scar by Acupuncture.” Journal of Acupuncture and Tuina Science 9, no. 3 (June 2011): 159–61. https://doi.org/10.1007/s11726-011-0499-z.
- Dunning, James, Raymond Butts, Firas Mourad, Ian Young, Sean Flannagan, and Thomas Perreault. “Dry Needling: A Literature Review with Implications for Clinical Practice Guidelines.” Physical Therapy Reviews 19, no. 4 (August 2014): 252–65. https://doi.org/10.1179/108331913X13844245102034.
- Langevin, Helene M., David L. Churchill, James R. Fox, Gary J. Badger, Brian S. Garra, and Martin H. Krag. “Biomechanical Response to Acupuncture Needling in Humans.” Journal of Applied Physiology 91, no. 6 (December 2001): 2471–78. https://doi.org/10.1152/jappl.2001.91.6.2471.
- Langevin, H. M., D. L. Churchill, and M. J. Cipolla. “Mechanical Signaling through Connective Tissue: A Mechanism for the Therapeutic Effect of Acupuncture.” FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology 15, no. 12 (October 2001): 2275–82. https://doi.org/10.1096/fj.01-0015hyp.
- Langevin HM, Langevin, Helene M., David L. Churchill, Junru Wu, Gary J. Badger, Jason A. Yandow, James R. Fox, and Martin H. Krag. “Evidence of Connective Tissue Involvement in Acupuncture.” The FASEB Journal 16, no. 8 (June 2002): 872–74. https://doi.org/10.1096/fj.01-0925fje.
- Langevin, Helene M., Elisa E. Konofagou, Gary J. Badger, David L. Churchill, James R. Fox, Jonathan Ophir, and Brian S. Garra. “Tissue Displacements during Acupuncture Using Ultrasound Elastography Techniques.” Ultrasound in Medicine and Biology 30, no. 9 (September 1, 2004): 1173–83. https://doi.org/10.1016/j.ultrasmedbio.2004.07.010.
- Langevin, Helene M., Nicole A. Bouffard, Gary J. Badger, David L. Churchill, and Alan K. Howe. “Subcutaneous Tissue Fibroblast Cytoskeletal Remodeling Induced by Acupuncture: Evidence for a Mechanotransduction-Based Mechanism.” Journal of Cellular Physiology 207, no. 3 (June 2006): 767–74. https://doi.org/10.1002/jcp.20623.
- Langevin, Helene M., Nicole A. Bouffard, David L. Churchill, and Gary J. Badger. “Connective Tissue Fibroblast Response to Acupuncture: Dose-Dependent Effect of Bidirectional Needle Rotation.” The Journal of Alternative and Complementary Medicine 13, no. 3 (April 2007): 355–60. https://doi.org/10.1089/acm.2007.6351.
- Julias, Margaret, Lowell T Edgar, Helen M Buettner, and David I Shreiber. “An in Vitro Assay of Collagen Fiber Alignment by Acupuncture Needle Rotation.” BioMedical Engineering OnLine 7, no. 1 (2008): 19. https://doi.org/10.1186/1475-925X-7-19
- Perreault, T, M T Grubb, B C Gendron, J C Perez, and S O Flannagan. “Mechanisms and Dose Parameters of Manual Needle Stimulation: Clinical Considerations – Part 2.” Acupuncture in Physiotherapy, 2019, 15.