Trigger Finger
Trigger finger is one of the most prevalent causes of hand disability 1. About 2.6% of the population will suffer from trigger finger across their life span2. Although trigger finger is considered a mild hand pathology, it has a wide-ranging impact on hand functioning, daily activities and quality of life 3. It can be caused by trauma or inflammation that causes a narrowing of the A1 pulley and flexor tendon thickening, causing pain, clicking, catching, and loss of motion of the affected finger 4.
Recent Evidence of Dry Needling Treatment of Trigger Finger
A recent article written by Azizian et al, demonstrates the mechanotransductive effects of dry needling on collagen networks in tendon pulley architechture5. In this RCT they randomized patients with trigger finger and the intervention group received a single session of dry needling. A needle inserted into the skin over the nodule and driven into the tendon in the A1 pulley anatomic location. One minute of needle manipulation was performed. Before intervention, pain DASH score, pully-tendon thickness and pinch grip were measured. One week later, these outcomes were measured using the same method. Pain and pinch grip were measured by visual analog scale and digital hand dynamometer. The DASH is a 30-item questionnaire measuring the patient’s functional status during the preceding week. Tendon-pully architecture was measured using an ultrasonography device assessing the A1 pully thickness and tendon cross-section. Results showed that the thickness of pulley-tendon decreased, pinch grip power increased, and DASH questionnaire score was decreased in comparison to the control group. They concluded that a single session of Dry Needling was effective in decreasing pain, DASH score, pulley-tendon thickness and improving pinch grip power in patients with trigger finger. But this change in tendon architecture and thickness is a clear example of mechanotransducive qualities of dry needling and its effect physiologically on collagen fiber orientation and density.
Mechanotransduction – What is it?
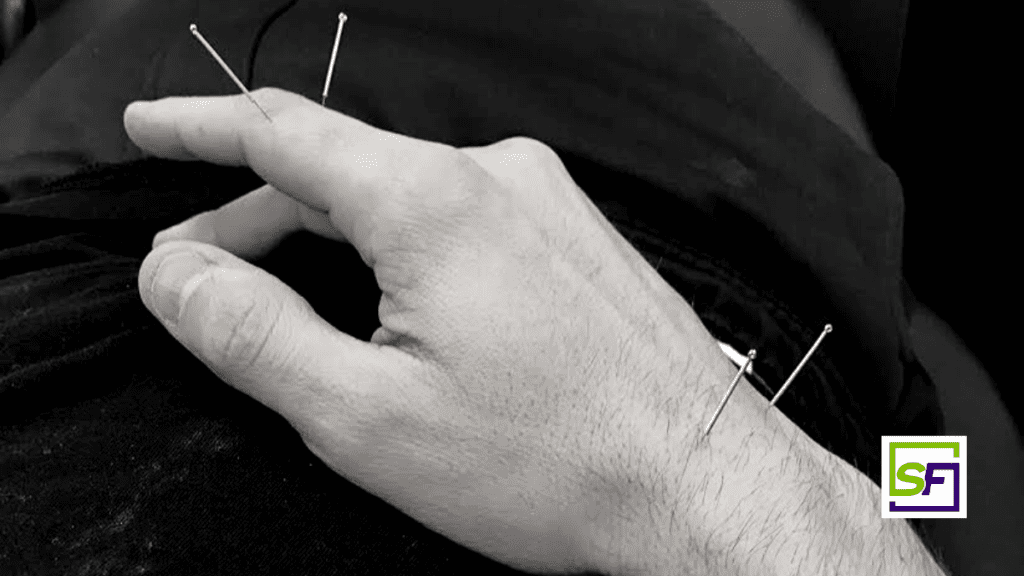
During dry needling, therapist’s use fine needles that may be manipulated manually, typically by either pitoning or needle rotation. This creates the biomechanical phenomenon experienced by the therapist known as needle grasp. In needle grasp, the therapist feels a resistance to further needle manipulation or rotation6. This, however, transmits a mechanical stimulus at the cellular level described in the literature as mechanotransduction.
What is occurring physiologically?
A series of recent studies by Langevin et al., describes what is occurring during mechanotransduction and the mechanism’s involved7-12. These articles suggest that needle grasp results when collagen fibers and other tissues wind around the rotating needle8-12. The tissues experience significant deformation during this process and induces a remodeling by fibroblastic activity11-12. Thus, this mechanotransducive mechanism is driven by tissue deformation through needle manipulation to mechanically stimulate fibroblasts for therapeutic benefits7-9. These ideas were also verified by Julias et al. who explored this link between tissue properties and collagen fiber winding13.
Conclusion
In addition to the article reviewed above, there is plenty of research that supports the fact that dry needling can impact collagen density and the healing of the tissues in animal studies14-18. There is also additional evidence for its use on tendon pulley architecture in humans19. A comprehensive discussion of these mechanism’s and responses to the mechanical stimulus of dry needling can be found in Perreault et al6. This information informs how we use dry needling for the purposes of healing and remolding of tissues, scars, etc.
Brian Hortz, PhD, AT, SFDN
Director of Research and Education – Structure & Function Education
Sue Falsone PT, MS, SCS, ATC, CSCS, COMT, RYT®
Owner – Structure & Function Education
To learn more about the Pentamodal Method
If you’re interested in learning how Structure & Function Education’s Pentamodal Method of of dry needling can be used to manipulate tissue healing, enroll today in the Foundations in Dry Needling for Orthopedic Rehab & Sport Performance (SFDN1) at www.structureandfunction.net.
References:
- Mardani Kivi, Mohsen, Farivar Abdullahzadeh Lahiji, Ali Babaei Jandaghi, Khashayar Saheb Ekhtiari, and Keyvan Hashemi Motlagh. “Efficacy of Sonographically Guided Intra-Flexoral Sheath Corticosteroid Injection in the Treatment of Trigger Thumb.” Acta Orthopaedica Et Traumatologica Turcica 46, no. 5 (2012): 346–52. https://doi.org/10.3944/aott.2012.2787.
- Akhtar, Sohail, Mary J. Bradley, David N. Quinton, and Frank D. Burke. “Management and Referral for Trigger Finger/Thumb.” BMJ (Clinical Research Ed.) 331, no. 7507 (July 2, 2005): 30–33. https://doi.org/10.1136/bmj.331.7507.30.
- Langer, Danit, Adina Maeir, Michael Michailevich, and Shai Luria. “Evaluating Hand Function in Clients with Trigger Finger.” Occupational Therapy International 2017 (January 10, 2017). https://doi.org/10.1155/2017/9539206.
- Makkouk, Al Hasan, Matthew E. Oetgen, Carrie R. Swigart, and Seth D. Dodds. “Trigger Finger: Etiology, Evaluation, and Treatment.” Current Reviews in Musculoskeletal Medicine 1, no. 2 (June 2008): 92–96. https://doi.org/10.1007/s12178-007-9012-1.
- Azizian, Morteza, Hossein Bagheri, Gholam Olyaei, Azadeh Shadmehr, Mohammad Ali Okhovatpour, Pooneh Dehghan, Shohreh Jalaei, and Hadi Sarafraz. “Effects of Dry Needling on Tendon-Pulley Architecture, Pain and Hand Function in Patients with Trigger Finger: A Randomized Controlled Trial Study.” Journal of Physical Therapy Science 31, no. 4 (2019): 295–98. https://doi.org/10.1589/jpts.31.295.
- Perreault, T, M T Grubb, B C Gendron, J C Perez, and S O Flannagan. “Mechanisms and Dose Parameters of Manual Needle Stimulation: Clinical Considerations – Part 2,” 2019, 15.
- Langevin, Helene M., David L. Churchill, James R. Fox, Gary J. Badger, Brian S. Garra, and Martin H. Krag. “Biomechanical Response to Acupuncture Needling in Humans.” Journal of Applied Physiology 91, no. 6 (December 2001): 2471–78. https://doi.org/10.1152/jappl.2001.91.6.2471.
- Langevin, H. M., D. L. Churchill, and M. J. Cipolla. “Mechanical Signaling through Connective Tissue: A Mechanism for the Therapeutic Effect of Acupuncture.” FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology 15, no. 12 (October 2001): 2275–82. https://doi.org/10.1096/fj.01-0015hyp.
- Langevin HM, Langevin, Helene M., David L. Churchill, Junru Wu, Gary J. Badger, Jason A. Yandow, James R. Fox, and Martin H. Krag. “Evidence of Connective Tissue Involvement in Acupuncture.” The FASEB Journal 16, no. 8 (June 2002): 872–74. https://doi.org/10.1096/fj.01-0925fje.
- Langevin, Helene M., Elisa E. Konofagou, Gary J. Badger, David L. Churchill, James R. Fox, Jonathan Ophir, and Brian S. Garra. “Tissue Displacements during Acupuncture Using Ultrasound Elastography Techniques.” Ultrasound in Medicine and Biology 30, no. 9 (September 1, 2004): 1173–83. https://doi.org/10.1016/j.ultrasmedbio.2004.07.010.
- Langevin, Helene M., Nicole A. Bouffard, Gary J. Badger, David L. Churchill, and Alan K. Howe. “Subcutaneous Tissue Fibroblast Cytoskeletal Remodeling Induced by Acupuncture: Evidence for a Mechanotransduction-Based Mechanism.” Journal of Cellular Physiology 207, no. 3 (June 2006): 767–74. https://doi.org/10.1002/jcp.20623.
- Langevin, Helene M., Nicole A. Bouffard, David L. Churchill, and Gary J. Badger. “Connective Tissue Fibroblast Response to Acupuncture: Dose-Dependent Effect of Bidirectional Needle Rotation.” The Journal of Alternative and Complementary Medicine 13, no. 3 (April 2007): 355–60. https://doi.org/10.1089/acm.2007.6351.
- Julias, Margaret, Lowell T Edgar, Helen M Buettner, and David I Shreiber. “An in Vitro Assay of Collagen Fiber Alignment by Acupuncture Needle Rotation.” BioMedical Engineering OnLine 7, no. 1 (2008): 19. https://doi.org/10.1186/1475-925X-7-19
- Almeida, Marcos dos Santos, Letícia Prado Oliveira, Cristiano Pedrozo Vieira, Flávia Da Ré Guerra, and Edson Rosa Pimentel. “Birefringence of Collagen Fibres in Rat Calcaneal Tendons Treated with Acupuncture during Three Phases of Healing.” Acupuncture in Medicine 34, no. 1 (February 2016): 27–32. https://doi.org/10.1136/acupmed-2015-010845.
- Almeida, Marcos dos Santos de, Andréa Aparecida de Aro, Flávia Da Ré Guerra, Cristiano Pedrozo Vieira, Benedicto de Campos Vidal, and Edson Rosa Pimentel. “Electroacupuncture Increases the Concentration and Organization of Collagen in a Tendon Healing Model in Rats.” Connective Tissue Research 53, no. 6 (December 1, 2012): 542–47. https://doi.org/10.3109/03008207.2012.710671.
- Almeida, Marcos dos Santos de, Karine Moura de Freitas, Letícia Prado Oliveira, Cristiano Pedrozo Vieira, Flávia Da Ré Guerra, Mary Anne Heidi Dolder, and Edson Rosa Pimentel. “Acupuncture Increases the Diameter and Reorganisation of Collagen Fibrils during Rat Tendon Healing.” Acupuncture in Medicine 33, no. 1 (February 2015): 51–57. https://doi.org/10.1136/acupmed-2014-010548.
- Park, Sang In, Yun-Young Sunwoo, Yu Jin Jung, Woo Chul Chang, Moon-Seo Park, Young-An Chung, Lee-So Maeng, et al. “Therapeutic Effects of Acupuncture through Enhancement of Functional Angiogenesis and Granulogenesis in Rat Wound Healing.” Evidence-Based Complementary and Alternative Medicine 2012 (2012): 1–10. https://doi.org/10.1155/2012/464586.
- Wang, Fan, Guang-wei Cui, Le Kuai, Jian-min Xu, Ting-ting Zhang, Huai-jin Cheng, Hong-sheng Dong, and Gui-rong Dong. “Role of Acupoint Area Collagen Fibers in Anti-Inflammation of Acupuncture Lifting and Thrusting Manipulation.” Evidence-Based Complementary and Alternative Medicine 2017 (2017): 1–8. https://doi.org/10.1155/2017/2813437.
- Inoue, Motohiro, Miwa Nakajima, Tatsuya Hojo, Megumi Itoi, and Hiroshi Kitakoji. “Acupuncture for the Treatment of Trigger Finger in Adults: A Prospective Case Series.” Acupuncture in Medicine 34, no. 5 (October 2016): 392–97. https://doi.org/10.1136/acupmed-2016-011068.