If I learned anything throughout my dry needling experiences, it’s this: all needling techniques are not created equal for all patients. These small instruments make a mighty impact on the body’s muscular, skeletal, endocrine and nervous systems and, when used properly, can yield incredible results in a short amount of time. However, using needles effectively requires intimate knowledge of anatomy and physiology as well as hands-on experience. To help you use needling as an agent for positive patient outcomes, I’d like to introduce you to a handful of dry needling techniques and give you guidelines on how to decide which kind is best for each unique patient.
How to Choose the Best Dry Needling Method
Every evidence-based treatment intervention has a time and a place, and it’s important to choose a tool based on the patient in front of you. Before I choose which type of dry needling to utilize, I first consider my Pentamodal Method of Dry Needling and analyze if dry needling is even the appropriate avenue of treatment. Use the three P’s to cover all of the factors that dictate if dry needling is right for your patient:
- Practitioner: Are you, the practitioner, trained and experienced in dry needling? Are you confident in your ability to use the tool to cause positive change?
- Patient: Is your patient comfortable with the idea of dry needling? Do they have any symptoms or conditions that would disqualify them from being needled safely? Do they have any contraindications or precautions that would prevent you from needling them, or give you pause on using dry needling as an intervention?
- Pathology: Is your patient presenting with a well-defined condition that can be affected through a form of dry needling?
If the answer to any of these is “no,” consider choosing an alternative method of treatment or attend a CEU course to learn how to dry needle safely and effectively. If the answer to those questions is “yes,” refer to the following list of dry needling techniques to find which type has the best chance of delivering your (and your patient’s) desired results.
6 Types of Dry Needling You Need to Know
Trigger Point
Trigger point dry needling is just what it sounds like; when your patient’s pain stems from an active trigger point, you can use a needle to directly address that single spot until it releases (Gattie et al, 2017). If your patient’s pain generator is an active trigger point, trigger point dry needling would be a very effective method of dry needling.
- Risk: Medium – If a trigger point is not the pain generator, this type of dry needling will not be effective, and you’ll need to choose another method.
- Needle Length: Depends on the depth of muscle that is being treated, the size of the patient and any anatomical risk factors in the area being treated. Could range anywhere from 25 mm to 125 mm.
- Example Use Case: If a patient’s myofascial pain in his or her neck is caused by a trigger point in the upper trapezius, trigger point dry needling can relieve these pain symptoms.
Superficial
Superficial dry needling (Baldry 2002; Griswold, 2019) is commonly used by many hands-on healthcare professionals. The needle is only inserted a few millimeters into the skin, reaching the epidermal layer but avoiding the muscle or bone. This method of needling targets the sensorimotor system: the needle changes the sensory input, therefore changing the motor output. Pain can be significantly altered as well.
- Risk: Low – Because the needle is not penetrating many layers of the body, there is a significantly lower opportunity to cause damage to vital organs or neurovascular structures.
- Needle Length: Typically, a short needle, only a few millimeters in length is needed. Ranges are typically from .3mm to 10mm.
- Example Use Case: In precarious areas like the thoracic spine, for example, clinicians run the risk of high risk of puncturing a lung if the needle is inserted too deeply. Superficial dry needling is a great way to change or alter this patient’s pain perception while avoiding the potential of injury.
Deep
Deep dry needling (Ceccherelli et al 2002; Boluk 2016; Fernández-Carnero et al 2017) is a higher-skilled method of needling that targets the muscle directly. In some areas of the body, manually manipulating a particular muscle can be challenging depending on the location of the target muscle and the tissues that are surrounding the target muscle. Deep dry needling allows clinicians to get into the target muscle to create a change in pain perception, impact scar tissue or relax/ decrease tightness.
- Risk: High – Just like exercise therapy, laser, ultrasound and other interventions, deep dry needling can be dangerous if you aren’t incredibly knowledgeable about human anatomy. Only attempt this type of needling if you’re experienced and have a great respect and understanding of the surrounding anatomy .
- Needle Length: 15mm-125mm (depending on the target structure)
- Example Use Case: If a patient’s piriformis muscle is incredibly tight and causing sciatic nerve pain, deep dry needling can be used to get past the glute muscles and tissue and decrease piriformis tightness, therefore decreasing sciatic pain.
Periosteal Pecking
Periosteal pecking involves using a dry needle to actually peck at the bone in an attempt to help with healing (Dunning et al, 2018). This triggers neuroendocrine responses which, when done intracapsularly, can help from those dealing with painful osteoarthritis symptoms. Hyaluronic acid production, anti-inflammatory processes and increases in endogenous opioid levels are other reasons why we think periosteal pecking is effective, specifically in knee osteoarthritis.
- Risk: High – Inserting a needle into the joint capsule carries risk. Surgical implants and infection risk factors need to be considered for each patient.
- Needle Length: Deep enough to get close to or down to the bone. Length will vary based on the size of the patient and area being needled.
- Example Use Case: If a patient with knee osteoarthritis is experiencing pain, use periosteal pecking, with or without electrical stimulation, in and around the knee joint in order to alter pain perception in the area and help stimulate chemical reactions that can help kickstart the healing process.
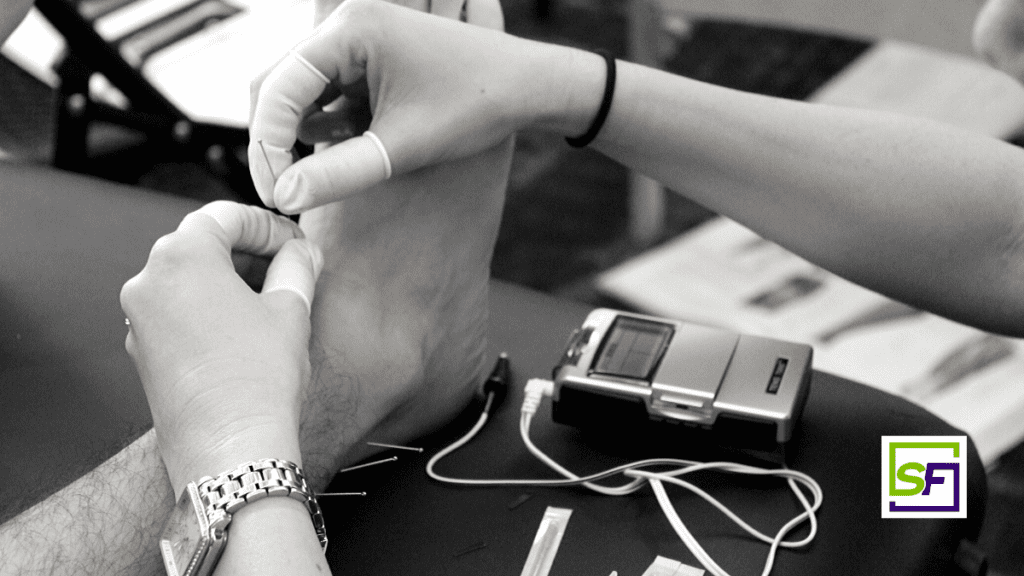
Electrical Stimulation
Adding electrical stimulation to the needles is a specialized form of dry needling. The addition of electrical stimulation triggers a neuroendocrine response that is different than needles alone (Butts and Dunning 2016, Perreault et al 2018). This form of dry needling taps into different pain modulation centers and pathways in the central nervous system, making it a possible choice for chronic pain patients and patients with osteoarthritis.
- Risk: Moderate – Certain conditions are contraindicated to using electrical stimulation, such as patients with pacemakers. The associated risk of other systemic issues must be taken into account on an individual basis.
- Needle Length: Deep – There is not enough purchase of the epidermis with superficial needling to attach electrical stimulation, so the needle must be in the muscle at least, or even down to the bone if using the electrical stimulation to carry out periosteal pecking.
- Example Use Case: See Periosteal Pecking above.
Peripheral Neuromodulation
Peripheral neuromodulation is beyond the scope of practice for most orthopedic healthcare professionals and should only be performed by a licensed acupuncturist or a western medical practitioner with internal medicine education (Longhurst and Tjen-A-Looi, 2013). This complicated and dynamic form of needling is used to affect organs, but the mechanism behind this concept can be activated any time you insert a needle. We do not get to choose what is being affected when a needle is inserted into a patient; the body will do with the stimulus what it will, meaning a systemic reaction is always a possibility when needling, even if it is not the desired result.
It’s no secret that organ pain can cause somatic pain – chest pain comes standard with a heart attack, and back pain is common with kidney stones. However, this is not a one-way street. The connection also goes the opposite way, which means that it is possible to use a needle within the somatic system to address organ issues or systemic issues.
When I insert a needle in someone, let’s say in an arm, I’m not just needling the brachialis muscle (as an example). I’m also needling the C5/C6 dermatome and affecting these spinal segments, which means anything else that’s innervated by C5/C6, including any organs or muscles, is also going to be affected.
- Risk: High – While you can use needles to affect certain change, ultimately the nervous system chooses what’s going to be affected. This increases the risk for autonomic nervous system reactions, such as changes in blood pressure or heart rate.
- Needle Length: Variable, depending on the structure being targeted.
- Example Use Case: When acupuncturists are treating conditions like asthma, high blood pressure, or anxiety, peripheral neuromodulation concepts are used.
Want to learn about the evidence behind each method of dry needling and get interactive experience? Structure & Function Education’s weekend-long CEU courses will give you an opportunity to master the fundamentals or sharpen your advanced needing skills.
References:
- Baldry P. Superficial versus deep dry needling. Acupuncture in Medicine. 2002;20(2-3):78-81.
- Boluk, Huma. “Comparision of Two Different Dry-Needling Techniques in the Treatment of Myofascial Pain Syndrome.” Ağrı – The Journal of The Turkish Society of Algology, 2016.
- Butts R, Dunning J. Peripheral and Spinal Mechanisms of Pain and Dry Needling Mediated Analgesia: A Clinical Resource Guide for Health Care Professionals. International Journal of Physical Medicine & Rehabilitation. 2016;04(02).
- Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L. Comparison of Superficial and Deep Acupuncture in the Treatment of Lumbar Myofascial Pain: A Double-Blind Randomized Controlled Study. The Clinical Journal of Pain. 2002;18(3):149-153.
- Dunning J, Butts R, Young I, et al. Periosteal Electrical Dry Needling as an Adjunct to Exercise and Manual Therapy for Knee Osteoarthritis. The Clinical Journal of Pain. 2018:1.
- Fernández-Carnero, Josué, Laura Gilarranz-de-Frutos, Jose Vicente León-Hernández, Daniel Pecos-Martin, Isabel Alguacil-Diego, Tomás Gallego-Izquierdo, and Aitor Martín-Pintado-Zugasti. “Effectiveness of Different Deep Dry Needling Dosages in the Treatment of Patients with Cervical Myofascial Pain: A Pilot RCT.” American Journal of Physical Medicine & Rehabilitation 96, no. 10 (October 2017): 726–33.
- Gattie E, Cleland JA, Snodgrass S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 2017;47(3):133-149.
- Griswold, D., M. Wilhelm, M. Donaldson, K. Learman, and J. Cleland. “The Effectiveness of Superficial versus Deep Dry Needling or Acupuncture for Reducing Pain and Disability in Individuals with Spine-Related Painful Conditions: A Systematic Review with Meta-Analysis.” Journal of Manual & Manipulative Therapy 27, no. 3 (May 27, 2019): 128–40.
- Longhurst JC, Tjen-A-Looi S. Acupuncture Regulation of Blood Pressure. International Review of Neurobiology Neurobiology of Acupuncture. 2013:257-271.
- Perreault, T, S O Flannagan, M T Grubb, and R Grubb. “Mechanisms and Dose Parameters of Electric Needle Stimulation: Clinical Considerations – Part I.” Acupuncture in Physiotherapy, 2018, 10.